Your leg muscle strength can shape how you move, stand, and feel today. When your leg muscle works well, your daily life feels lighter. You are not chasing energy, you are building it.
You do not need extreme plans, you need steady practice and calm consistency. With the right focus, your muscles learn balance and comfort.
Why leg muscle strength feels like daily energy

Your leg muscle system supports your whole body. It carries you through stairs, errands, and long days. It also supports maintaining posture when you sit and stand.
When your muscles get stronger, movement feels smoother. You often notice less pain in the knee, hip, and ankle. You also feel steadier when you turn, stop, and start.
A strong leg muscle helps you move with confidence. It lowers injury risk during sports and normal chores. It also helps you protect your joints as you age.
A simple map of your upper and lower leg
Think of the upper and lower leg as a team with shared goals. The upper leg drives power, while the lower leg manages balance. Together, they guide every step of your leg.
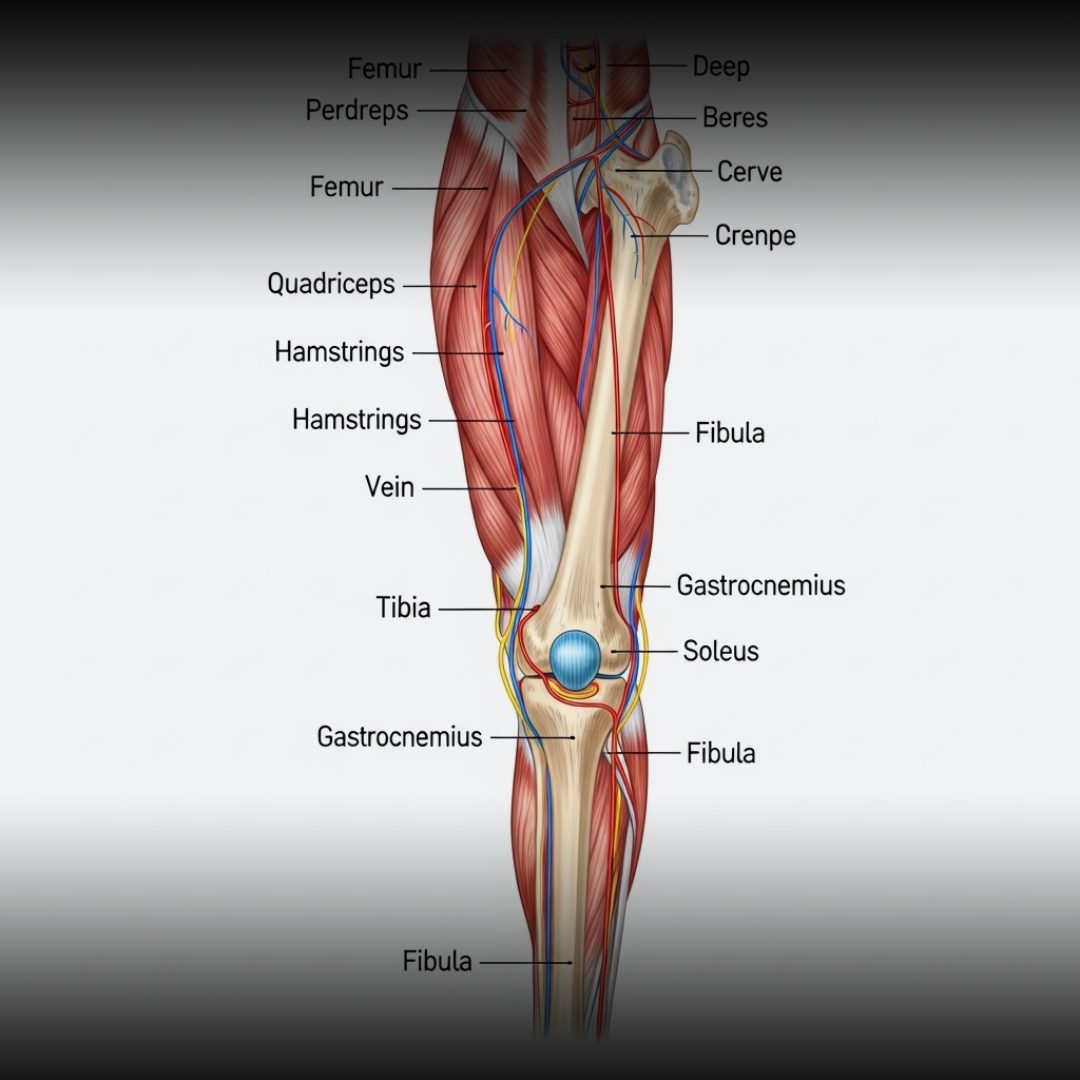
Your major muscle groups include the quadriceps, the hamstrings, and the calf. These muscle groups work with smaller stabilizers for clean movement. Even your foot control matters for safe walking.
If you enjoy anatomy, classic texts like gray's anatomy outline these ideas clearly. Still, you do not need a textbook mindset. You only need simple awareness and good habits.
The upper leg: power around the hip and thigh

Your upper leg wraps around the thigh and connects to the hip. The thigh bone supports this area like a strong column. When you train well, you protect both the hip and the knee.
The quadriceps are four muscles in the front of the thigh. They include the rectus femoris, the vastus medialis, and the vastus lateralis. These main muscles help extend the knee and control landing.
Your backside matters too. The hamstrings include the biceps femoris, and they support knee flexion. They also support hip extension when you rise from a chair.
The knee joint: stability you can trust
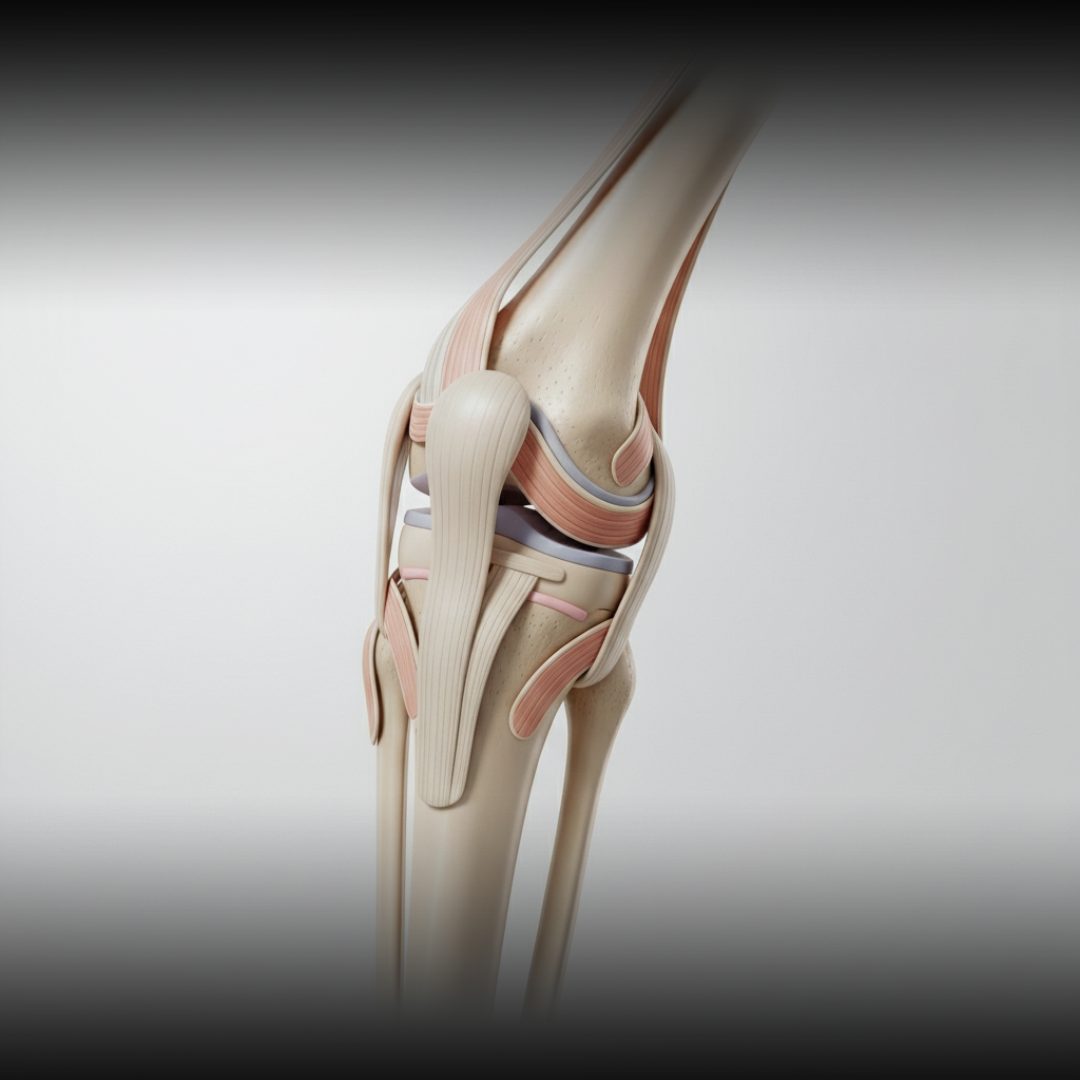
Your knee joint links the upper leg and the lower leg. It handles force every time you step, squat, or jump. When your muscles guide it well, your knee feels safe.
Strong quadriceps help keep the knee stable under load. Strong hamstrings reduce forward pull at the knee. This balanced control can lower your risk of common twists.
Pay attention to alignment during training. Keep the knee tracking over the foot. This supports good posture and reduces strain through the hip and ankle.
READ ALSO: Knee Therapy for Pain That Focuses on Long-Term Relief
The lower leg: spring, balance, and the foot

Your lower leg controls the foot and steadies your step. The lower leg muscles also help you handle uneven ground. This matters for safety, comfort, and speed.
Important movers include the tibialis anterior and the tibialis posterior. You also use the fibularis longus to support the arch and balance. Smaller helpers like the extensor digitorum longus and flexor digitorum longus guide toes.
When these muscles get tired, you may feel shaky. You might notice leg pain around the ankle or the top of the foot. You may even notice control issues like foot drop in rare cases.
READ ALSO: Bulgarian Split Squat Exercise For Calm Strength Training
Calf muscles and the achilles tendon connection

Your calf is a key engine in the lower leg. It supports walking, running, and quick direction changes. It also supports steady standing during long lines.
Your calf muscles work with the achilles tendon to push the foot down. The gastrocnemius has a lateral head that helps create power. When your calf is strong, your steps feel springy. If you feel tightness, take it seriously. Mild tightness can grow into calf pain. A calm recovery plan can reduce pain and restore comfort.
How to train without muscle strain

A strong leg muscle plan respects your recovery. You build strength, then you give your muscle tissue time to adapt. This is how you avoid repeated setbacks.
Most training setbacks come from speed, not effort. You add too much volume, and muscle strain shows up. You can also trigger overuse injuries when you skip rest. Start with a simple rhythm. Train your muscles, then rest, then train again. If you feel sharp pain, reduce load and move gently.
Warm-up and mobility that protect muscle tissue

A warm-up prepares your muscles and your joints. It also increases blood flow through key blood vessels. This can make your first set feel smoother. Begin with easy steps and gentle ranges. Use light squats, ankle circles, and hip swings. Keep your feet hip width apart for balance.
Add a short hinge drill to wake the back chain. Let the hamstrings bend slowly with control. This supports good mechanics and reduces muscle strain risk.
Strength moves you can do at home

You can build a strong leg muscle with simple moves. You only need your body weight and a little space. Focus on control and consistency. Try sit to stands, step ups, and wall sits for the thigh. Add slow lunges to train the front leg and the glutes. Keep your knee steady and use good form.
Add balance work on one leg for stability. You can also do calf raises for the calf and the lower leg. Finish with toe raises to support the top of the foot and the big toe.
READ ALSO: Home Gym Exercise Equipment That Fits Your Flow
Building a balanced leg muscle routine

Balance means you train the upper leg and the lower leg together. You also train the hip to guide the whole chain. This keeps your muscles working as one.
Aim for the three main muscles that move your steps, quadriceps, hamstrings, and calf. Then add support from the gluteus maximus and the gluteus medius. These are among the largest muscles in your lower body.
Remember the quads are four muscles, and each matters. Use squats for the quads and hinges for the hamstrings. Use slow raises to train the foot and ankle control.
Recovery habits that reduce pain and leg pain

Recovery is where your muscle fibers rebuild. Sleep helps the nervous system calm down and reset. When you rest well, strength returns faster.
Hydration supports circulation and cramp control. During heavy weeks, remember to stay hydrated. Better fluid balance supports the blood vessels that feed your working muscles.
Use easy walking on rest days for blood flow. Gentle stretching can ease the calf and the thigh. If you feel ongoing pain, reduce intensity and focus on technique.
When pain is not normal: red flags and health conditions

Some discomfort is normal after training. However, sudden swelling, warmth, or a heavy ache can signal health conditions. It is smart to check in with a clinician.
Be alert if you feel sudden severe pain in the calf with swelling. In rare cases, this can relate to deep vein thrombosis. This is urgent, especially with shortness of breath.
Also watch for numbness, weakness, or signs of nerve damage. Issues like persistent foot drop need care. If you notice other symptoms, do not ignore them.
Balanced legs, balanced life

Your leg is more than a tool for motion. It is a foundation for calm strength and steady energy. When your leg muscle works well, your whole day feels smoother.
Choose simple actions you can repeat. Train the main muscles with care, protect your joints, and respect recovery. Over time, your muscles will support your knee, your hip, and your ankle with ease. Keep going with kindness toward yourself. You are building strength that lasts. And you are creating balance that you can feel, step by step.
UP NEXT: Mindful Body Whispers the Path to Inner Balance






















